Physiology of Optic Disc
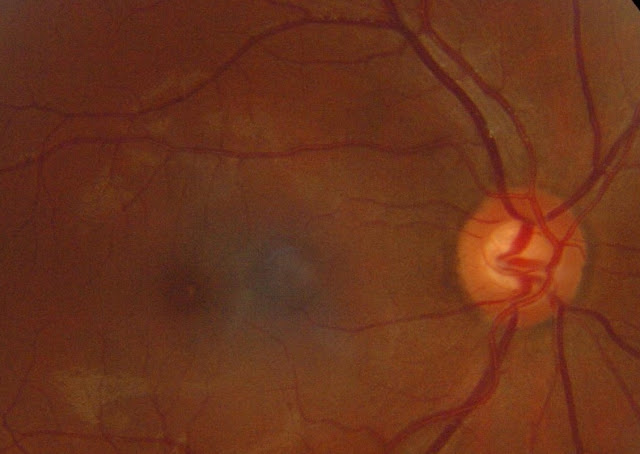
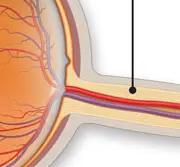
The optic disc, also known as the optic nerve head, is the point at which the optic nerve fibers leave the eye and enter the brain. The physiology of the optic disc is critical in understanding the normal functioning of the visual system and the causes and effects of eye diseases. Function of the Optic Disc The main function of the optic disc is to transmit visual information from the retina to the brain. The retina is the light-sensitive layer of tissue at the back of the eye that converts light into electrical signals. These electrical signals are then transmitted to the brain via the optic nerve. The optic disc is where the optic nerve fibers converge to form the optic nerve. The optic disc also plays an important role in maintaining the health of the retina. The blood vessels that supply the retina with blood and oxygen enter and exit the eye through the optic disc. The optic disc also contains a small number of retinal pigment epithelial cells that help to protect and support the